"When you have a chance to sit at the decision-making table, make sure you do not forget why you are there."
Dr. Okey K. Enyia, Founder & CEO
"When you have a chance to sit at the decision-making table, make sure you do not forget why you are there."
Dr. Okey K. Enyia, Founder & CEO
Enyia Strategies: Where Purpose Meets Policy
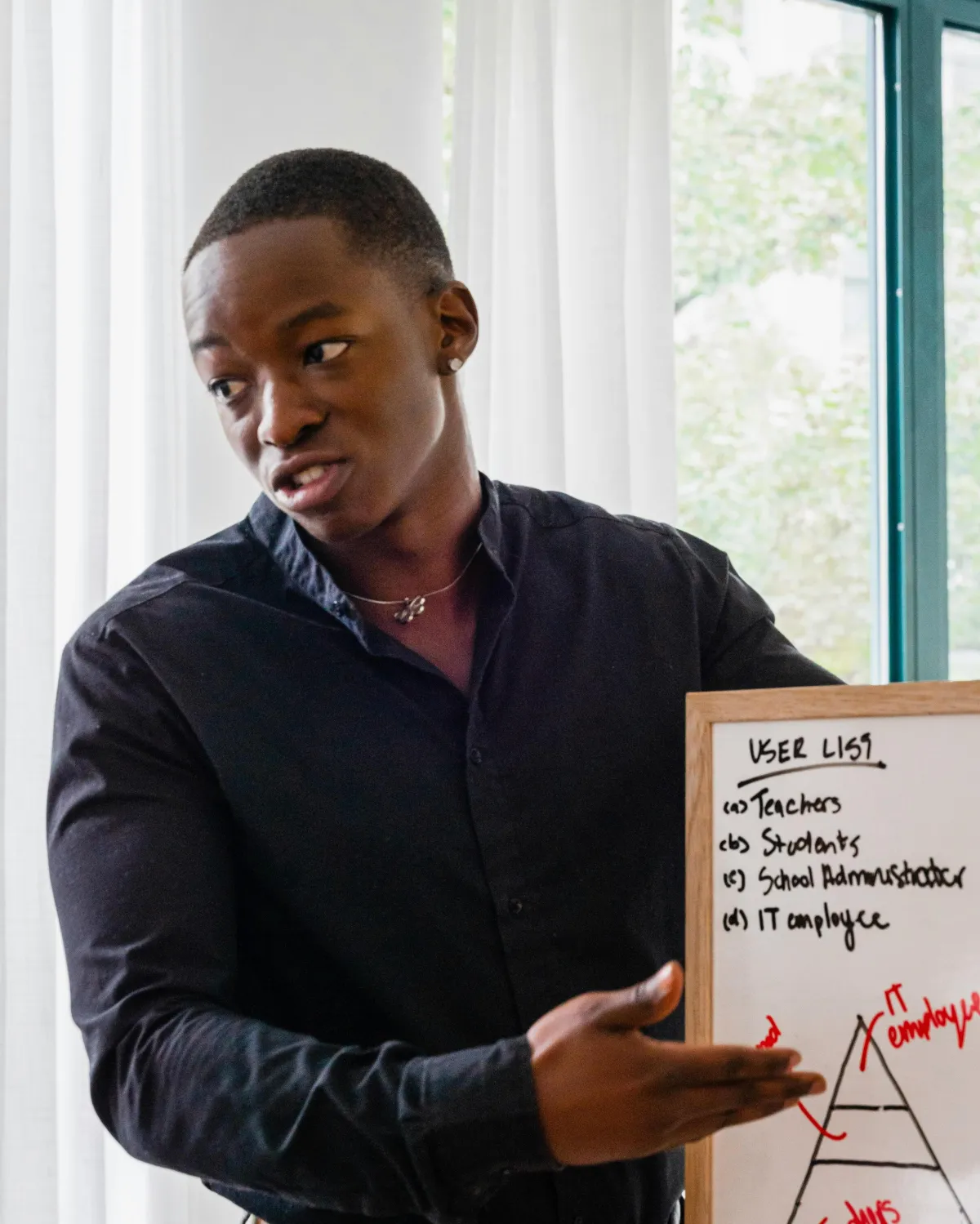
At Enyia Strategies, we transform bold ideas into measurable impact. We are a mission-driven policy advocacy consulting firm specializing in strategic advising, legislative strategy, and evidence-based research for clients working to advance health equity, social justice, and systemic change. Working at the intersections of government, policy, and community, we help organizations—from nonprofits and academic institutions to coalitions and corporations—navigate complex political landscapes, influence decision-makers, and drive meaningful reform.
Founded by Dr. Okey K. Enyia, a seasoned public health strategist, former congressional health policy advisor, and scholar-activist, Enyia Strategies brings over 15 years of experience at the nexus of health policy, government affairs, and advocacy. Our firm delivers tailored services including policy research and analysis, stakeholder engagement, campaign design, and capacity-building—all grounded in cultural humility, analytical precision, and a commitment to equity.
Whether you’re shaping legislation, launching a national campaign, or building power within underserved communities, Enyia Strategies is your strategic ally in delivering bold, forward-thinking solutions that are both visionary and actionable.
Enyia Strategies: Where Purpose Meets Policy
At Enyia Strategies, we transform bold ideas into measurable impact. We are a mission-driven policy advocacy consulting firm specializing in strategic advising, legislative strategy, and evidence-based research for clients working to advance health equity, social justice, and systemic change. Working at the intersections of government, policy, and community, we help organizations—from nonprofits and academic institutions to coalitions and corporations—navigate complex political landscapes, influence decision-makers, and drive meaningful reform.
Founded by Dr. Okey K. Enyia, a seasoned public health strategist, former congressional health policy advisor, and scholar-activist, Enyia Strategies brings over 15 years of experience at the nexus of health policy, government affairs, and advocacy. Our firm delivers tailored services including policy research and analysis, stakeholder engagement, campaign design, and capacity-building—all grounded in cultural humility, analytical precision, and a commitment to equity.
Whether you’re shaping legislation, launching a national campaign, or building power within underserved communities, Enyia Strategies is your strategic ally in delivering bold, forward-thinking solutions that are both visionary and actionable.
Educate. Empower.
Execute.
Enyia Strategies: Where Purpose Meets Policy

Service 1
Government affairs strategy and coalition development

Service 2
Keynote speaking and facilitation

Service 3
Policy advocacy workshops and campaign design
Service 4
Leadership coaching and thought partnership

Service 5
Brand storytelling and narrative strategy
Enyia Strategies: Where Purpose Meets Policy

Service 1
Strategic & Fractional Leadership

Service 2
Policy & Advocacy Design

Service 3
Thought Leadership & Media Engagement
Congressional Black Caucus Foundation
"Policy for the People" Health Equity Summit
Alpha Phi Alpha Fraternity, Inc., Annual Founder's Day on Capitol Hill
Policy Luncheons
Download: The Policy Power Playbook
Unlock the insider tips that Enyia Strategies uses to help mission-driven organizations influence legislation, move policy, and create lasting impact.

Featured Podcast Appearance
Episode 13: The Anointing of Only – Insights from Dr. Okey K. Enyia
on The Wise Counsel Project Podcast
Dr. Okey K. Enyia joins The Wise Counsel Project to explore the concept of “The Anointing of Only” — a powerful reflection on purpose, identity, and navigating leadership as the "only" in the room. In this insightful conversation, he shares personal stories, spiritual grounding, and practical encouragement for professionals called to serve in unique and often isolating spaces.
Stay Connected with Enyia Strategies
Want the latest insights, strategies, and updates delivered straight to your inbox? Join our email list and be the first to know about new content, events, and opportunities.
Download: "The Policy Power Playbook"
The Policy Power Playbook
Unlock the insider tips that Enyia Strategies uses to help mission-driven organizations influence legislation, move policy, and create lasting impact.
Enyia Strategies
Where Purpose Meets Policy
© 2026 Enyia Strategies - All Rights Reserved
